The Nursing Home Law Center is committed to providing the legal resources necessary to hold negligent facilities accountable.
Pressure Wound Care

Individuals who have limited mobility are in danger of developing pressure wounds. These sores are preventable but can lead to life-threatening conditions if untreated.
In this article, we’ll cover an overview of pressure wounds, how to care for a pressure injury, methods to prevent bedsores, and how you can hold nursing homes accountable if you or your loved ones develop pressure ulcers while under their care.
Nursing Home Law Center can help you navigate your legal options and get compensated for their negligence.
What are Pressure Wounds?
Pressure wounds have many names. They can be called pressure ulcers, bedsores, or decubitus ulcers. Pressure ulcers occur when your skin is exposed to prolonged pressure. The continuous pressure can damage the skin’s surface, underlying tissues, and, in severe cases, bones.
They are more likely to occur when people have limited or no mobility and are often confined to sitting in a bed or chair for long periods. Pressure sores can develop at any point on the body; however, the most common pressure ulcer sites are bony body areas with less fat and muscle padding. Common locations of pressure ulcers include:
- Heels and ankles
- Tailbone and hip
- Knees and elbows
- Back of the head and ears
- Shoulder blades
The longer the body remains unmoved, the deeper the decubitus ulcer can get.
Stages of Pressure Wounds
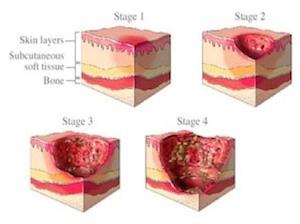
There are four stages of pressure wounds, each with unique characteristics that help medical professionals diagnose them.
- Stage 1: A stage 1 pressure sore is the least severe. They are often red, blue, or purple patches of skin that look almost like bruises. They can feel warm to the touch, and victims often complain of burning and itching sensations. Stage one pressure ulcers do not blanch with pressure and have not broken through the skin. If left untreated, these pressure ulcers can develop into deeper wounds.
- Stage 2: The skin has broken in stage 2 pressure injuries. They look like blisters, torn skin, or open wounds due to the partial-thickness skin loss. The damage has penetrated through the epidermis and dermis skin layers. The wound may be weeping and swollen, and the skin around the area may be discolored. It will be warm, itchy, and painful to touch. Because of the open skin, infection can easily set in the area.
- Stage 3: Stage 3 pressure ulcers extend beyond the surface level of the skin, penetrating the subcutaneous tissue or deeper. They look like skin craters, with black tissue (eschar) and slough (discolored slimy tissue) that can make it difficult to see in the wound. These pressure ulcers are often red, swollen, and filled with pus. They are warm and discolored around the edges. Stage 3 pressure ulcers can lead to cellulitis and other health complications if left untreated.
- Stage 4: Stage 4 pressure ulcers cause extensive tissue damage. Bones, muscles, tendons, ligaments, and joints can be exposed through the open wound, which can cause excruciating pain. It can have black or brown skin, with colored pus oozing from the wound. These pressure ulcers often have a foul odor. They can lead to cancer, sepsis, gangrene, amputation, and other life-threatening conditions.
There are also unstageable pressure ulcers when doctors cannot determine the ulcer’s severity. Slough and eschar can obstruct their view. They will need to remove the dead tissue to assess the severity of the injury.
When the injury is discovered, nursing homes should take immediate pressure ulcer prevention steps, including removing the external pressure. Treating pressure ulcers promptly is crucial to reduce risk factors for infection and other life-threatening complications.
Why Pressure Wounds Are a Serious Concern
Pressure wounds can have life-threatening health consequences, especially for the elderly and those with compromised immune systems. They can cause:
- Sepsis: A blood infection that can cause organ damage and failure, leading to death.
- Osteomyelitis: A bone infection that may require surgery to treat.
- Cellulitis: A bacterial infection that can cause swelling, inflammation, and redness in the area.
- Marjolin ulcer: A long-term non-healing wound that can lead to squamous cell carcinoma (cancer).
- Death: Patients with untreated chronic pressure ulcers can die from complications.
Pressure wounds also have a prolonged healing process, which means victims can suffer unduly as they recover from their pressure injuries. They severely impact a patient’s quality of life. It is painful to move, and the wound’s odor may cause them to self-isolate, leading to depression and anxiety.

Principles of Pressure Wound Healing
Unfortunately, pressure wounds are common in nursing homes. Patients can develop pressure injuries due to understaffing, underfunding, and poor care conditions. If you experience a pressure injury, here’s what you should know about pressure ulcer management.
Relieving Pressure Ulcers
When a pressure injury is identified, immediately relieve pressure on the infected area.
- Reposition the body to restore the blood flow.
- Use support surfaces like specialized mattresses and cushions to prevent pressure.
- Use offloading devices like boots to help redistribute the weight.
Do not place pressure on this fragile skin until the pressure ulcer is healed.
Wound Cleaning and Dressing
After the pressure has been relieved, cleanse the area that has bed sores. Saline solution or prescribed cleansers can help remove the infection and promote healing.
Specialized dressing may also be used, including:
- Hydrocolloids: These dressings help create a moist environment to heal pressure ulcers. They are also waterproof and reduce friction and shear forces.
- Alginates: These dressings are made from seaweed extracts and can help retain moisture to keep the pressure ulcer dry.
- Foams: Foam dressings help redistribute pressure, reduce moisture, and prevent friction from pressure injuries.
Specialized dressings can help speed up healing by preventing infection. They keep the wound dry and act as a barrier from continuous pressure.
Debridement
Debridement can help remove dead tissue from a pressure ulcer. This is necessary if there is a deep tissue injury. Depending on the severity of the wound, a doctor may choose to remove the dead tissue through various methods.
- Sharp: This is a surgical method in which a scalpel or scissors remove the dead tissue. It is often used if there is still healthy tissue around the pressure ulcer.
- Mechanical: High or low water pressure is used to remove the tissues.
- Enzymatic: An enzyme solution is applied to the pressure ulcer to help dissolve the tissue. It can also be applied via dressing.
- Autolytic: Doctors will add a moist wound dressing to help promote the body’s natural healing process.
Debridement is an effective way to speed up the healing process for pressure ulcers.
Infection Control
Oral antibiotics can be used to help treat infected pressure sores. Topical antibiotics can also be used if the wound is not healing after 14 days. Signs of infection include:
- Redness
- Swelling
- Tender
- Discharge or pus
- Foul odor
- Fever
- Pain
Antiseptics, antibiotics, and other antimicrobial treatments can help prevent the infection from spreading and treat the pressure ulcer.
Nutrition and Hydration
Proper nutrition and hydration can help promote wound healing. Your diet should include a mix of protein, vitamins, and minerals, including vitamin C, zinc, and copper.
A dietitian can help provide education and a meal plan to ensure you get enough calories and nutrients. You can take supplements to help you meet your minimum daily requirements.
Pain Management
It’s essential to manage pain while treating pressure wounds. Victims can take:
- Pain relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen can help mitigate pain.
- Topical solutions: Topical pain medication can be applied when changing wounds or during debridement
- Repositioning: Moving positions can also help relieve pain and restore blood flow
You want to do what you can to be comfortable as your pressure ulcer heals.
Specialized Pressure Wound Care
There are also specialized pressure wound care options available to help promote healing.
Negative Pressure Wound Therapy (NPWT)
Negative pressure wound therapy (NPWT) is a technique that uses negative pressure from a vacuum to promote healing. It can also be known as vacuum-assisted closure (VAC). The pressure helps:
- Reduce swelling and inflammation
- Improve blood flow and stimulate new tissue growth
- Remove fluid from the wound and help pull the edges together.
NPWT is an effective treatment for nonhealing wounds.
Hyperbaric Oxygen Therapy (HBOT)
HBOT involves entering a pressurized chamber to breathe oxygen. The increased air pressure helps the lungs absorb more oxygen than normal, which can help promote healing.
This increased oxygen flow helps the tissues surrounding pressure wounds heal and fight infection. Depending on the severity of the pressure ulcer, the treatment can last 30 minutes to 2 hours.
Skin Grafts and Flaps
Doctors may also recommend that patients undergo surgical procedures to heal pressure ulcers.
- Skin grafts are when donor skin is used to cover a pressure ulcer.
- Skin flaps are when healthy tissue near the wound is partially detached to help cover the wound.
These treatments are used in severe or non-healing pressure wounds.
Preventing Pressure Sores
Nursing homes and care facilities can use several techniques to prevent pressure ulcers.
Pressure Ulcer Risk Assessment

Risk assessment tools like the Braden Scale can help identify at-risk patients. Patients are scored in six categories, including sensory perception, skin moisture, activity level, mobility, friction and shear, and nutrition. Their scores are used to determine treatment plans to prevent pressure injuries.
Skin Care and Hygiene
Proper skin care and hygiene are essential in preventing pressure injuries. The skin should be:
- Clean: The area should be clean and free from dirt, debris, and other unsanitary conditions.
- Dry: Skin should be kept dry from sweat and other moisture. Wet skin can tear more easily.
- Moisturized: While skin should be dry, it should also be moisturized to help prevent it from getting dry and brittle. Dry skin can crack easily.
Additionally, patients who struggle with incontinence should be kept free of urine and feces, as these can also cause the skin to break down.
Regular Repositioning
Nursing homes should frequently reposition patients who have mobility challenges. Typically, they should be repositioned every 15 minutes to prevent pressure injuries. Medical professionals should set a turning schedule to help them properly care for patients.
Support Surfaces
Specialized mattresses and cushions can help redistribute pressure on the body and keep it at a 30-degree angle. This can help reduce pressure on at-risk areas and prevent pressure injuries.
Nutrition and Hydration
What patients eat and drink can also impact their skin health. At-risk individuals should take care to obtain adequate nutrition and hydration to help promote skin elasticity. Healthy skin can be less likely to develop pressure injuries.
Nursing Home Negligence and Pressure Wounds
If you develop pressure wounds and suspect nursing home negligence, a nursing home injury attorney can help you understand your legal options.
Failure to Provide Adequate Care
Pressure wounds can be a sign of neglect or inadequate care in a nursing home. They only develop if patients are left unmoving for long periods. The deeper the wound, the longer the patient was left unattended.
If pressure injuries develop, the nursing home may have failed to provide adequate patient care, and they can be held liable.
Holding Nursing Homes Accountable
You have several legal options to hold nursing homes accountable for pressure wound injuries. You can file complaints directly with your state health department, federal government, or nursing home. They will investigate the conditions and make recommendations for improvement as appropriate.
Additionally, you can sue a nursing home and recover compensation for pressure injuries. You must first prove negligence by establishing a duty of care and that they breached it. As a result, you developed pressure injuries and suffered damage as a result.
If you prove negligence, you may be able to recover costs for your medical bills, pain and suffering, emotional distress, and more.

Secure Expert Legal Representation!
Decubitus ulcers can develop as a result of negligence in nursing homes. The nursing facility breached its duty of care to its patients, and they should be held liable for their actions. Nursing Home Law Center can help you get justice for your pressure ulcers.Contact us at (800) 926-7565 or complete our online form to schedule your free consultation with a pressure injury attorney. We can explain your legal options and help you recover damages for your injuries.